Mismatched unrelated donors (MMUD) has improved access to hematopoietic cell transplantation (HCT) for underrepresented minority groups. However, MMUD HCT is historically associated with inferior outcomes primarily due to the increased risk of graft-versus-host disease (GvHD), when conventional calcineurin inhibitor-based GvHD prophylaxis is used. Post-transplant cyclophosphamide (PTCy) is an established and effective agent as part of GvHD prophylaxis post haploidentical HCT, which has been increasingly used in the matched donor HCT setting. To date, there have been no prospective studies reporting the efficacy of PTCy after peripheral blood stem cell (PBSC) MMUD HCT. Here, we conducted a pilot trial to estimate the GVHD-free relapse/progression-free survival (GRFS) at one-year post HCT and to evaluate the efficacy of PTCy as GvHD prophylaxis using either an ablative or reduced intensity conditioning regimen after PBSC MMUD HCT (NCT 03128359).
Patients with hematologic malignancies (n=38), who were ≤75 years old, had KPS of ≥70%, and were scheduled for HCT from a 7/8 HLA-matched (A-, B-, C-, and DR-) donor were eligible. Patients received myeloablative conditioning (MAC, n=19) using Fludarabine (90 mg/m2) and FTBI (1200 cGy), or reduced intensity conditioning (RIC, n=19) using Fludarabine (100 mg/m2) and Melphalan (140 mg/m2 or 100 mg/m2 if >60 years old). All patients received GCSF-mobilized PBSC as the graft source. GvHD prophylaxis consisted of PTCy (50mg/kg x2 days), Tacrolimus (1mg/d), and MMF (1g x3/d).
Overall, patients' median age at HCT was 53 years (range: 21-72), and 50% were male. HCT indication was AML (n=17), ALL (n=8), MDS (n=6), CML (n=3), NHL (n=3), or CLL (n=1). DRI was low in 18 (47%), intermediate in 14 (37%) and high/very high in 6 (16%) patients. At HCT, 29 patients were in complete remission and 9 had active disease (Median BM blast: 3.4, range: 0-7). HCT-CI was >2 in 17 patients (45%). Donors (median age: 32 years, range: 19-53) were mismatched at HLA-A (n=15), -B (n=12), -C (n=8), or DR-loci (n=5) with the median number of mismatches of 2 (range: 1-4) out of 12. The median CD34+ cell dose was 5.45×106/kg (range: 2.39-9.35).
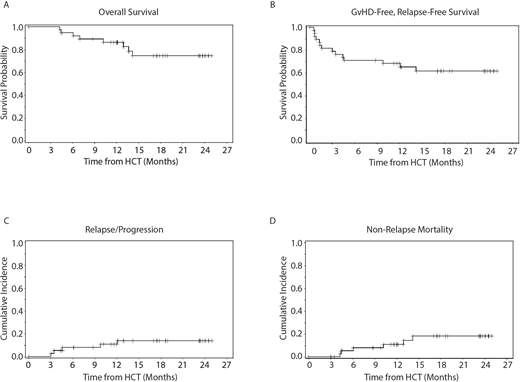
Median time to neutrophil engraftment was 16 days (range: 13-35). Complete donor chimerism (>99% if PCR or 95% if STR) was achieved in 36 patients (95%) by day 30 ± 7 days. With a median follow-up period of 18.1 months (range: 4.6 - 25.0), 1-year overall survival (OS) and GRFS were 87% (95% CI: 71-94) and 68% (95% CI: 51-81), respectively (Figure). Non-relapse mortality and relapse rate at 1 year were 11% (95% CI:4-27) and 11% (95% CI: 4-27), respectively (Figure). Cumulative incidence of day 100 acute GvHD grade 2-4 and 3-4 were 51% (95% CI: 38-70) and 19% (95% CI: 10-37), respectively. By NIH criteria, 1-year chronic GvHD was 52% (95% CI: 37-72) with moderate/severe chronic GvHD in 3% (95% CI 0.4-19). By exploratory post-hoc univariable analysis, RIC (vs. MAC) and intermediate/high-risk DRI (vs. low risk) were associated with worse GRFS (HR=4.7, 95%CI: 1.3-16.8, p=0.01 and HR=3.8, 95%CI: 1.1-13.8, p=0.04, respectively). The class and number of HLA mismatch, CD34+ cell dose, and absolute lymphocyte count were not predictive of GRFS. Infectious complications from Day -9 to +100 included CMV viremia (n=16) respiratory infections (n=5, 2 patients with lower respiratory), and BK virus cystitis (n=5). Fifteen patients had bacteremia (6 with GNR) and 4 had C. difficile colitis.
Correlative flow-cytometry data was available for 29 patients. T cells reconstitution (>300/ul) was seen in 17 patients (59%) by day 100 (n=11) or day 180 (n=6). NK cell recovery (>150/ul) was seen in 24 patients (85.7%) by day 28 (n=9), day 100 (n=11), or day 180 (n=4). NK cells were predominantly highly cytotoxic CD3-CD56dim. Regulatory T cell counts on day 30 was associated with GRFS: median: 0.20/ul (range: 0.04-2.21) in the group with GRFS event (n=8) compared with 0.68/ul (range: 0.08-23.0, p=0.03) in the group with no GRFS event (n=19).
Our pilot trial showed highly promising OS/GRFS in patients receiving PBSC MMUD HCT, indicating that PTCy is an effective GvHD prophylaxis platform in this setting. Our data support further development of PTCy in MMUD HCT to improve the access to and outcome of HCT in patients with hematologic disorders who have otherwise no suitable donor.
Al Malki:Neximmune: Consultancy; Rigel Pharma: Consultancy; Jazz Pharmacuticals, Inc: Consultancy. Ali:Incyte Corporation: Consultancy. Stein:Amgen: Consultancy, Speakers Bureau; Stemline: Consultancy, Speakers Bureau. Marcucci:Merck: Other: Research Support (Investigation Initiated Clinical Trial); Takeda: Other: Research Support (Investigation Initiated Clinical Trial); Novartis: Speakers Bureau; Pfizer: Other: Research Support (Investigation Initiated Clinical Trial); Abbvie: Speakers Bureau; Iaso Bio: Membership on an entity's Board of Directors or advisory committees. Nakamura:Merck: Other: advisory board meeting; NapaJen Pharma: Consultancy; Kadmon Corporation: Other: Advisory board meeting; Kyowa-Kirin: Other: Support on a meeting presentation; Alexion: Other: Support on a meeting presentation; Celgene: Other: Support on seminar; Magenta Therapeutics: Other: Advisory board meeting; Viracor: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.